Provider Resources & FAQ
No action required until June 30, 2023
How can I create a new Ameritas provider portal account?
If you don't have a provider portal account with Ameritas, log in to your portal at dentalselect.com to create your new Ameritas portal account. Use your Ameritas source code from an Ameritas EOP and follow the prompts to register. If you don't know your Ameritas source code, contact customer service at 800-999-9789 or customercare@ameritas.com
What can I find on the Ameritas portal regarding patient benefits?
On the Ameritas portal, you can access updated patient benefit information. This includes viewing pretreatment estimates and claim status for claims submitted on or after June 30.
Have the fee schedules changed?
Yes, the fee schedules have been streamlined for easier use. There is one Gold fee schedule for both copay and coinsurance plans, and one Platinum fee schedule for both copay and coinsurance plans. Specialists have one schedule for both Gold and Platinum. You can find these fee schedules on the new Ameritas portal. Updated Dental Select fee schedules will be sent annually.
Where can I find the Dental Select network directories?
You and your patients can find Dental Select network directories on the Find a Provider page at ameritas.com. Dental Select dental plan customers will access their member portal at ameritas.com.
Will patients have new ID cards and policy numbers?
Yes, patients with Dental Select insurance will receive new ID cards that show their network, new policy number and member ID, billing address, and plan information. A sample ID card is included in this information.
How can I appeal a claim? Has this process changed?
The internal CSR appeal form will no longer be used. To appeal, visit ameritas.com and search "appeals" for information on state-specific appeals rights. Requests for claim review should be sent to Quality Control at PO Box 82657, Lincoln, NE 68501-2657. Phone: 877-897-4328, Fax: 402-309-2579.
Has the timely filing period for claims changed?
Yes, the timely filing period for claims has changed from one year to 90 days or as the state requires.
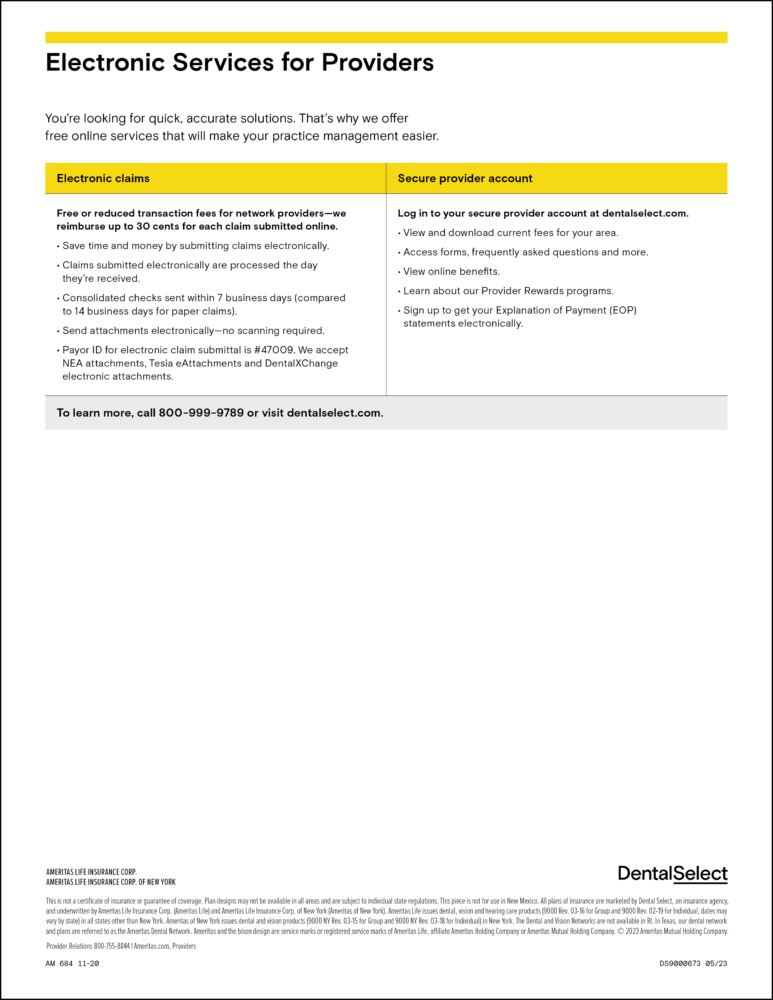
Can I still submit claims electronically?
Yes, you can still submit claims electronically. Ameritas will track electronic claims submissions and pay 30 cents per electronic claim each quarter once the $75 threshold is met.
What other changes should I be aware of regarding claims?
The claims address and payor ID changed. To streamline claims processing, you will submit claims to one address and one payor ID regardless of the plan type. The new claims address is PO Box 82520 Lincoln, NE 68501, and the new payor ID is 47009.
What other changes might I see?
You will see the Ameritas logo and contact information on your explanation of payments (EOPs) for Dental Select plans. Dental Select network materials, such as fee schedules and the provider guide, will continue to use the Dental Select brand. Updated forms can be found at dentalselect.com/forms.
Are there any additional advantages I should be aware of?
Yes, as a dentist working directly with Ameritas, you can take advantage of the Ameritas Provider Rewards program. This includes various savings programs and discounts to improve your practice's bottom line. Refer to the remaining information enclosed in this PDF.
When will these changes take place?
The changes will occur on June 30th, 2023.
Who can I contact if I have questions?
Please contact us via email at customercare@ameritas.com or by phone at 800-999-9789, Monday through Friday, 7 a.m. to 5 p.m. MT.